- Research
- Open access
- Published:
The serum soluble ASGR1 concentration is elevated in patients with coronary artery disease and is associated with inflammatory markers
Lipids in Health and Disease volume 23, Article number: 89 (2024)
Abstract
Background and aims
Current research has suggested that asialoglycoprotein receptor 1 (ASGR1) is involved in cholesterol metabolism and is also related to systemic inflammation. This study aimed to assess the correlation between the serum soluble ASGR1 (sASGR1) concentration and inflammatory marker levels. Moreover, the second objective of the study was to assess the association between sASGR1 levels and the presence of coronary artery disease (CAD).
Methods
The study subjects included 160 patients who underwent coronary angiography. Ninety patients were diagnosed with CAD, while seventy age- and sex-matched non-CAD patients served as controls. We measured the serum sASGR1 levels using an ELISA kit after collecting clinical baseline characteristics.
Results
Patients with CAD had higher serum sASGR1 levels than non-CAD patients did (P < 0.0001). sASGR1 was independently correlated with the risk of CAD after adjusting for confounding variables (OR = 1.522, P = 0.012). The receiver operating characteristic (ROC) curve showed that sASGR1 had a larger area under the curve (AUC) than did the conventional biomarkers apolipoprotein B (APO-B) and low-density lipoprotein cholesterol (LDL-C). In addition, multivariate linear regression models revealed that sASGR1 is independently and positively correlated with high-sensitivity C-reactive protein (CRP) (β = 0.86, P < 0.001) and WBC (β = 0.13, P = 0.004) counts even after adjusting for lipid parameters. According to our subgroup analysis, this relationship existed only for CAD patients.
Conclusion
Our research demonstrated the link between CAD and sASGR1 levels, suggesting that sASGR1 may be an independent risk factor for CAD. In addition, this study provides a reference for revealing the potential role of sASGR1 in the inflammation of atherosclerosis.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is a fatal disease with a complex etiology worldwide. Over the last few decades, there has been constant updating and even subversion of the understanding of atherosclerosis [1]. In parallel, an increasing number of atherosclerotic markers have been discovered [2, 3]. Disorders of lipid metabolism, especially hypercholesterolemia, are well-known pathogenic risk factors for ASCVD [4]. Lipoproteins are the initial points of interest. Oxidized low-density lipoprotein (ox-LDL) or small dense LDL enters the artery wall, which constitutes the classic early stage of atherosclerosis [2, 5]. Of course, circulating adhesion molecules such as vascular cell adhesion molecule-1 (VCAM), intercellular adhesion molecule-1 (ICAM), and monocyte chemotactic protein-1 (MCP-1) play crucial roles in this stage [5, 6]. High triglyceride (TG) and residual cholesterol levels are important pathogenic factors of ASCVD and were recognized when residual cardiovascular risk associated with statins was discovered [7, 8]. Other lipoproteins, such as lipoprotein(a) [Lp(a)] and apolipoprotein B (APO-B), have also been found to be associated with the risk of atherosclerosis [5]. Evaluating the characteristics of coronary artery plaques using the latest invasive or noninvasive imaging methods can help predict the risk of cardiac events and guide personalized treatment strategies [9,10,11]. A higher plaque burden and high risk plaques are independent risk factors for myocardial ischemia [11,12,13]. In addition, recent studies have established that inflammatory markers participate in all stages of atherosclerosis, making them one of the most promising therapeutic targets for treating this disease [14, 15].
Asialoglycoprotein receptor (ASGR) is a hepatic C-type lectin that is expressed mainly on the sinusoidal surface of hepatocytes [16, 17]. The primary function of ASGR is to bind glycoproteins containing terminal galactose or GlcNAc residues (such as asialoglycoproteins) in circulation [18, 19]. The complex is subsequently internalized under the coat of clathrin and transported to the lysosome for degradation [20]. As a hepatocyte membrane receptor, asialoglycoprotein receptor 1 (ASGR1) regulates hepatic cholesterol homeostasis by interacting with circulating asialoglycoproteins [21]. In animal studies, inhibiting hepatic ASGR1 or its binding to circulating asialoglycoproteins reduces serum cholesterol levels by promoting cholesterol efflux into the bile [21]. ASGR1 loss-of-function mutations are linked to a 0.4 mmol/l decrease in circulating non-high-density lipoprotein cholesterol (non-HDL-C) and a 34% reduction in the incidence of coronary artery disease (CAD) [22]. Notably, the effect of the ASGR1 mutation on the risk of CAD is significantly greater than that on non-HDL-C levels, suggesting that the significant reduction in the risk of CAD is not entirely explained by the effect of ASGR1 mutations on non-HDL-C levels [22, 23]. Therefore, ASGR1 mutations may be involved in other protective mechanisms than the regulation of cholesterol homeostasis, such as inflammation. Indeed, some direct or indirect evidence has shown that ASGR1 is involved in biological processes related to systemic inflammation and vascular inflammation [24,25,26,27]. For example, proinflammatory cytokines upregulate the expression of ASGR1 [24]. The interaction of ASGR1 with epidermal growth factor receptor (EGFR) activates the extracellular signal-regulated kinase (ERK) pathway [25], which has been linked to inflammatory regulation and atherosclerosis [28, 29]. However, the relationship between ASGR1 and inflammation in patients with CAD is unclear.
In contrast to ASGR1, which is located on the liver surface mentioned above, serum soluble ASGR1 (sASGR1), which is secreted by the liver, is another splicing variant of liver ASGR1 and is located in the circulation due to the absence of a transmembrane domain [30]. However, current research on sASGR1 is very limited. Although our previous study showed that sASGR1 is associated with LDL-C levels [31], the relationship between sASGR1 levels and the risk of CAD is still unclear.
C-reactive protein (CRP) levels and white blood cell (WBC) counts are the most basic and widely used indicators of systemic inflammation. In addition, CRP levels are positively correlated with the degree of coronary artery stenosis in patients with CAD [32]. Two recent studies have established that high-sensitivity C-reactive protein (hs-CRP) levels exhibit superior predictive power for future cardiovascular events and mortality risk when compared to circulating cholesterol levels in patients receiving statin therapy [33, 34]. Similarly, WBC counts have been widely confirmed to be closely related to atherosclerosis and CAD [35,36,37]. Currently, there are no simple or effective methods for determining the level of ASGR1 expression on the hepatocyte membrane in clinical practice. Therefore, the purpose of this study was to assess the correlation between sASGR1 levels and inflammatory marker levels, including hs-CRP levels, WBC counts, and WBC subsets. Moreover, the second objective of the study was to assess the association between sASGR1 levels and the presence of CAD.
Materials and methods
Study population
We consecutively included 160 patients admitted to the Second Xiangya Hospital of Central South University between September 2022 and September 2023 in this study. All patients underwent coronary angiography. Patients were categorized into two groups based on the results of coronary angiography: 90 patients with CAD and 70 patients without CAD. We matched the groups for age and sex. Four experienced angiographers performed coronary angiography, two of whom evaluated the vessels. To determine the severity of CAD, CAD patients were further subdivided into acute myocardial infarction (AMI) (n = 26) and CAD without AMI (n = 64) groups. The severity of coronary lesions was determined by the number of major coronary artery stenoses, which were classified as vessels ≤ 2 (n = 51) or vessels > 2 (n = 39). Furthermore, the Gensini score was also calculated to assess the severity of CAD. We excluded patients with infections, autoimmune diseases, liver diseases, renal failure, malignancies, or other serious diseases.
The diagnosis of CAD was based on angina pectoris manifestations, electrocardiogram changes, and coronary angiography, which indicated that the major vessel had a degree of stenosis greater than or equal to 50%. Elevated plasma troponin levels, together with evidence of acute myocardial ischemia, are diagnostic criteria for AMI [38]. Fasting blood glucose levels ≥ 126 mg/dl (7.0 mmol/L) or 2-hour postprandial blood glucose levels ≥ 200 mg/dL (11.1 mmol/L) were used to diagnose type 2 diabetes mellitus (T2DM). Repeated measures of blood pressure greater than or equal to 140/90 mmHg were used to diagnose hypertension.
The study was authorized by the ethics committee of Second Xiangya Hospital, which also found that it adhered to the ethical principles of the Declaration of Helsinki. Informed permission was obtained from all patients.
Sample size calculation
In the study assessing the association between sASGR1 levels and the presence of coronary artery disease (CAD), we used Power Analysis and Sample Size (PASS) software for sample size calculations. We set bilateral α = 0.05 and power = 0.9. The ratio of the sample size between the CAD group and the control group was 1.28:1. We set the mean and standard deviation of the sASGR1 levels for the two groups based on our preliminary results. The sample size calculation revealed that a sample of 55 CAD patients and 43 non-CAD patients achieved 90.31% power to reject the null hypothesis of equal means when the population mean difference was µ1- µ2 = 4–2.1 = 1.9 with standard deviations of 4 for the CAD group and 1.3 for the non-CAD group. Ultimately, 90 CAD patients and 70 non-CAD patients composed the sample.
Clinical characteristics and laboratory measurements
Basic information, including age, sex, body mass index (BMI), smoking status, and statin use, was collected and recorded. Peripheral blood samples were collected from patients through the elbow vein after they had fasted overnight. The serum was collected after centrifuging the blood sample for 10 min at 3,000 rpm and subsequently stored at -80 °C. Serum lipid parameters and hs-CRP levels were measured using a fully automated biochemical analyzer. WBCs, neutrophils, lymphocytes, and monocytes were counted using an automatic blood cell counter.
ELISA for determining the sASGR1 concentration
The serum concentration of sASGR1 was determined using sandwich enzyme-linked immunosorbent assay (ELISA) kits (JL41965; Jianglai Biology, Shanghai). Two measurements were repeated per sample to reduce random variations. Both the intraplate and interplate coefficients of variation (CVs) were less than 10%, suggesting that the assay has good repeatability. The recovery rate and linearity of this reagent kit were 95% and 91%, respectively (with a dilution ratio of 1:2). The minimum detectable concentration of serum sASGR1 was 0.156 ng/mL.
Statistical analyses
For the data analysis, we employed SPSS 25.0 statistical software. In addition, EmpowerStats statistical software (version 4.1) and R language (version 4.2.0) were used for subgroup analysis and interaction testing. P = 0.05 was used as the statistical criterion.
The continuous variables are displayed as the mean ± standard deviation or as medians and quartiles (Q1-Q3), and group comparisons were conducted using the independent-samples t test or Mann‒Whitney U test according to the type of data distribution. Chi-square tests were used to compare differences among categorical variables, which are presented as frequencies or percentages. The data were analyzed for a normal distribution by the D’Agostino–Pearson omnibus normality test. The Kruskal‒Wallis test was used to assess the association between sASGR1 levels and the severity of CAD. A multivariate logistic regression model was used to identify the factors that influence the presence of CAD. The diagnostic value of sASGR1 and traditional biomarkers in patients with CAD was assessed using receiver operating characteristic (ROC) curves. To further analyze the relationship between sASGR1 and inflammatory markers, we employed a stepwise multivariate regression model in which inflammatory markers were used as the dependent variables. For subgroup analysis, stratified linear regression models were employed, and likelihood ratio tests were applied to find any variations or interactions.
Results
Baseline characteristics
The basic details and biochemical characteristics of the study subjects are listed in Table 1. BMI, smoking status, statin use, history of hypertension, and T2DM status were greater in the CAD group than in the non-CAD group (P < 0.05). The CAD group had higher serum TG, LDL-C, Lp(a), APO-B, and hs-CRP levels; WBC and neutrophil counts; and monocyte counts than did the non-CAD group (P < 0.05). HDL-C levels were greater in non-CAD patients (P < 0.05). There were no significant differences in age, sex, lymphocyte count, or other blood lipid parameters between the two patient groups.
Serum sASGR1 levels in the CAD and non-CAD groups
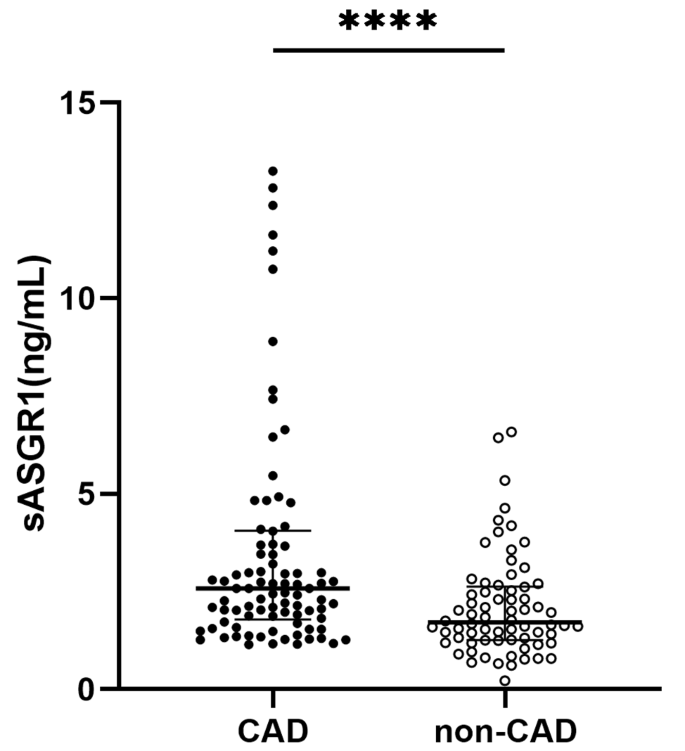
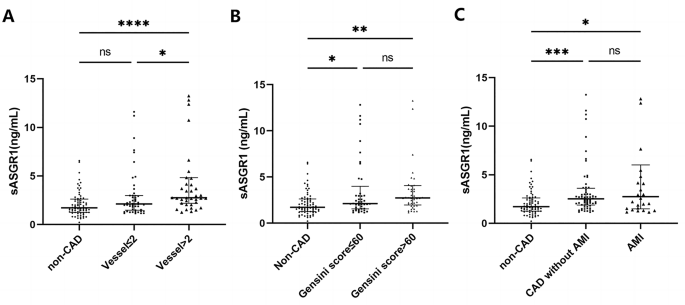
As shown in Fig. 1, the serum level of sASGR1 in CAD patients was significantly greater than that in non-CAD patients [2.58 (1.8, 4.1) vs. 1.71 (1.3, 2.6) ng/ml, P < 0.0001]. Subsequently, we investigated the relationship between sASGR1 levels and the severity of CAD. As shown in Fig. 2A, a lack of significant difference was observed between CAD patients with ≤ 2 diseased vessels and non-CAD patients [2.12 (1.5, 3.0) vs. 1.71 (1.3, 2.6) ng/ml, P = 0.078]. However, the level of sASGR1 in CAD patients with > 2 diseased vessels was significantly greater than that in non-CAD patients [2.76 (2.2, 4.8) vs. 1.71 (1.3, 2.6) ng/ml, P < 0.0001] or in CAD patients with ≤ 2 diseased vessels [2.76 (2.2, 4.8) vs. 2.12 (1.5, 3.0) ng/ml, P = 0.033]. Additionally, we separated patients into two groups according to the median (60) Gensini score to assess the association between sASGR1 level and CAD severity more precisely: Gensini score ≤ 60 (n = 45) and Gensini score > 60 (n = 45). However, there was no significant increase in the level of sASGR1 as the Gensini score increased (Fig. 2B). In addition, we were unable to identify significant differences in the severity of CAD between individuals with and without AMI (Fig. 2C).
The relationship between sASGR1 levels and the severity of CAD. (A) sASGR1 levels in patients with different CAD statuses and numbers of involved vessels. Comparisons were evaluated by the Kruskal‒Wallis test. ns, not statistically significant. *P < 0.05. ****P < 0.0001. For vessels ≤ 2, the number of involved vessels was < 2; for vessels > 2, the number of involved vessels was more than 2. (B) Comparison of sASGR1 levels in patients with different Gensini scores. Comparisons were evaluated by the Kruskal‒Wallis test. ns, not statistically significant. *P < 0.05. **P < 0.01. (C) sASGR1 levels in patients with different severities of CAD. Comparisons were evaluated by the Kruskal‒Wallis test. ns, not statistically significant. *P < 0.05. ***P < 0.001
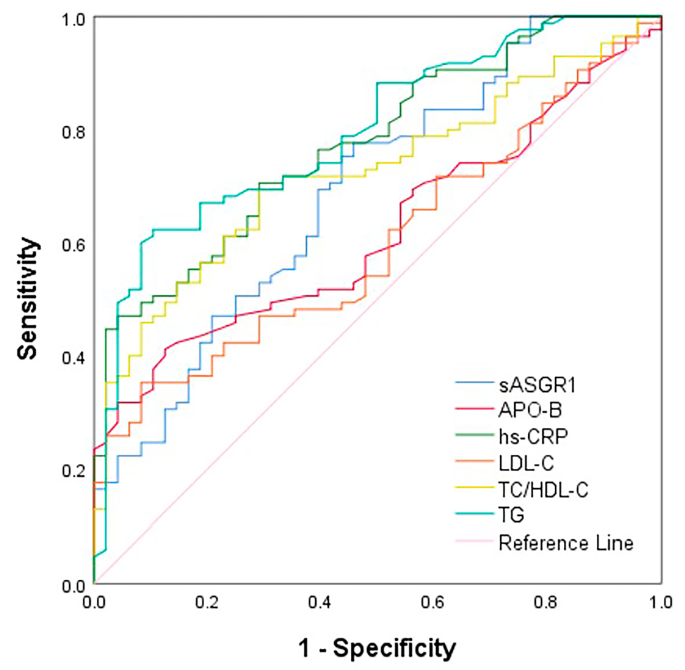
Diagnostic value of sASGR1 and traditional biomarkers for CAD patients
We used receiver operating characteristic (ROC) curves to evaluate the diagnostic ability of sASGR1 levels for CAD (Fig. 3). The area under the curve (AUC) of sASGR1 was 0.691 (95% CI = 0.60–0.78, P < 0.001). Its diagnostic utility was better than that of the traditional biomarkers APO-B (AUC: 0.619, 95% CI: 0.53–0.71, P = 0.023) and LDL-C (AUC: 0.599, 95% CI: 0.50–0.69, P = 0.059), despite not being comparable to that of hs-CRP (AUC: 0.775, 95% CI: 0.70–0.85, P < 0.001), TG (AUC: 0.796, 95% CI: 0.72–0.87, P < 0.001), or total cholesterol (TC)/high-density lipoprotein cholesterol (HDL-C) (AUC: 0.723, 95% CI: 0.64–0.81, P < 0.001). sASGR1 has a cutoff value of 1.682 ng/ml for predicting the occurrence of CAD, with a sensitivity of 77.6% and a specificity of 54.2%. The sensitivity and specificity of the other biomarkers for predicting the presence of CAD were as follows: hs-CRP (sensitivity: 47.1%, specificity: 95.8%), APO-B (sensitivity: 41.2%, specificity: 87.5%), LDL-C (sensitivity: 35.3%, specificity: 91.7%), TC/HDL-C (sensitivity: 69.4%, specificity: 70.8%), and TG (sensitivity: 62.4%, specificity: 89.6%).
sASGR1 is an independent influencing factor for the occurrence of CAD
A multivariate logistic regression model was used to identify the factors that influence the presence of CAD. We included independent variables based on the results of univariate analysis, clinical significance, sample size, and multicollinearity. The results showed that sASGR1, smoking, TG, hypertension, and T2DM were associated with an increased risk of CAD after controlling for BMI, smoking status, TG, LDL-C, hs-CRP, hypertension, and T2DM (Table 2). For every unit increase in the sASGR1 level, the risk of CAD increased by 0.52 times (OR = 1.522, 95% CI = 1.095, 2.115; P = 0.012).
Relationships between the serum sASGR1 concentration and inflammatory marker level
By setting hs-CRP levels, WBC counts, and WBC subsets as dependent variables, we used stepwise multivariate regression models to determine the correlation between sASGR1 levels and inflammatory marker levels (Table 3). After we adjusted for sex, age, BMI, smoking status, statin use, hypertension status, T2DM status, and CAD status (Model II), sASGR1 was positively associated with the levels of inflammatory markers [hs-CRP (β = 1.00, p < 0.001), WBC count (β = 0.12, P = 0.004), and neutrophil count (β = 0.09, P = 0.011)]. Given that previous research has indicated a link between blood lipid levels and inflammation [39], we further adjusted for blood lipid parameters and found that the serum sASGR1 concentration was significantly positively correlated with the serum hs-CRP level (β = 0.86, P < 0.001), WBC count (β = 0.13, P = 0.004), and neutrophil count (β = 0.10, P = 0.008). Additionally, a similar association was observed between sASGR1 concentration and monocyte count (β = 0.009, P = 0.014).
Subgroup analysis of the correlation between sASGR1 and inflammatory marker levels
According to the interaction test (Table 4), the effect of sASGR1 on the hs-CRP level was significantly affected by age (p for interaction = 0.015), sex (p for interaction = 0.007), BMI (p for interaction = 0.002), and hypertension status (P for interaction = 0.019), indicating that the association between the sASGR1 concentration and the hs-CRP level differed according to these variables. Notably, even after we adjusted for factors such as age, sex, BMI, statin use, smoking status, and lipid parameters, the positive correlation between sASGR1 and hs-CRP levels was still significant in patients with CAD (β = 0.8, P < 0.001). Among patients without CAD, this correlation was not observed (P = 0.231).
Similarly, we also conducted subgroup analysis and interaction testing to determine the relationship between sASGR1 and WBC count. Age was the sole significant factor influencing the association between sASGR1 level and WBC count, in contrast to hs-CRP (P for interaction < 0.001), as shown in Table 5. Interestingly, similar to that of hs-CRP, a positive correlation between sASGR1 and WBC was observed only in CAD patients (β = 0.1, P = 0.029).
Discussion
According to our study, sASGR1 is independently and positively correlated with hs-CRP and WBC. According to our subgroup analysis, this relationship existed only for CAD patients. In addition, serum sASGR1 levels are elevated in CAD patients. sASGR1 is independently correlated with the risk of CAD after adjusting for confounding variables, and it has better diagnostic value than APO-B and LDL-C.
Since 2016, ASGR1 has received widespread attention from researchers due to its involvement in liver cholesterol metabolism [22]. Recent animal studies have shown that inhibiting ASGR1 on the hepatocyte membrane (named hASGR1) is expected to become a new strategy for reducing LDL-C levels [21]. Similarly, genetically mimicked ASGR1 inhibitors were associated with lower cholesterol levels and CAD risk [40]. In addition, an observational study showed that ASGR1 mRNA levels in peripheral blood mononuclear cells were lower in CAD patients than in non-CAD patients, but the underlying mechanism is still unknown [23]. However, there is currently no research on the role of serum sASGR1 in CAD patients. sASGR1 and LDL-C levels were found to be positively correlated in our recent study [31]. As expected, this study showed an increase in sASGR1 levels in CAD patients, which is consistent with the findings of a recent study [41]. In the present study, plasma proteomics analysis revealed ASGR1 to be a risk factor for ischemic heart disease. Thus, the results of our study lend support for sASGR1 as a potential biomarker for CAD. We also found that, after controlling for confounding variables, sASGR1 remained an independent risk factor for CAD (Table 2). As mentioned earlier, hASGR1 regulates liver cholesterol homeostasis by binding to circulating asialoglycoproteins, ultimately affecting plasma cholesterol levels and the risk of CAD [21, 22]. Previous research revealed that while sASGR1 inhibits the binding of circulating asialoglycoproteins to hASGR1, it still binds to asialoglycoproteins and enters the liver as a complex [30, 31]. Taken together, these findings imply that the entry of the sASGR1-asialoglycoprotein complex into hepatocytes may exert similar downstream biological effects as the binding of the asialoglycoprotein to hASGR1. Another hypothesis, however, is that the serum sASGR1 concentration might reflect the hASGR1 protein level. Given this, it will be intriguing to investigate whether blocking sASGR1 can lower plasma cholesterol and the risk of CAD in a manner similar to inhibiting hASGR1.
We evaluated the relationship between serum sASGR1 levels and the severity of CAD. Although the serum sASGR1 concentration was associated with the number of coronary artery lesions (Fig. 2A), the level of sASGR1 did not significantly increase as the Gensini score increased (Fig. 2B). The serum sASGR1 concentration has been reported to be positively correlated with LDL-C levels [31], but the correlation between LDL-C level and Gensini score is not significant [42, 43]. The relationship between serum sASGR1 levels and the severity of CAD in this study remains uncertain, even though the Gensini score is a more accurate indicator of plaque burden and CAD severity than the number of vascular lesions. More precise methods, such as intravascular ultrasound and optical coherence tomography, may be needed to evaluate the relationship between sASGR1 and the severity of CAD. We failed to find that sASGR1 could be used to identify individuals who had an AMI (Fig. 2C). Our previous study showed that there is no correlation between the serum troponin T concentration and sASGR1 level [31], which is consistent with the results of this study, indicating that the sASGR1 level is not related to the degree of myocardial injury.
We analyzed the diagnostic value of the sASGR1 level for CAD. Although it does not have the same diagnostic efficacy as hs-CRP, it is superior to LDL-C and APO-B. In addition, sASGR1 has advantages over hs-CRP (47.1%), APO-B (41.2%), TG (62.4%), and TC/HDL-C (69.4%) due to its relatively high diagnostic sensitivity (77.6%), indicating an advantage in the early screening of CAD.
In addition to its clear association with cholesterol metabolism, a small number of studies have shown that ASGR1 is associated with systemic inflammation. The most direct evidence shows that knockdown of Asgr1 in mouse liver and monocytes suppressed the expression of plasma inflammatory cytokines [interleukin-1 (IL-1), IL-6, and tumor necrosis factor (TNF-α)] [27]. However, these studies on the relationship between ASGR1 and systemic inflammation have focused mainly on the role of ASGR1 as a hepatocyte or monocyte membrane receptor. The relationships between serum sASGR1 levels and inflammatory marker levels in healthy individuals and patients with disease are unknown. Our findings showed that the serum sASGR1 concentration is positively correlated with inflammatory marker levels (hs-CRP and WBC), which supports and propels previous basic research. However, the causal link between sASGR1 and inflammatory markers warrants further exploration.
Inflammation is a key factor in the development of atherosclerosis and CAD. As a stable and reliable inflammatory marker, CRP has been shown to upregulate the expression of adhesion molecules and monocyte chemokines, inhibit the production of endothelial nitric oxide synthase (eNOS), and promote arterial thrombosis, indicating direct involvement in the occurrence of atherosclerosis [44,45,46]. Therefore, evaluating hs-CRP levels is highly important for CAD patients without hypercholesterolemia, as there is no urgent demand for lipid-lowering agents. The CANTOS study identified for the first time the ability of anti-inflammatory treatment to reduce cardiovascular events, which was independent of blood lipid levels [47]. An association between plasma CRP and LDL-C levels has been demonstrated in previous research [39]. Despite the fact that ASGR1 does affect circulating cholesterol levels, our subgroup analysis results showed that sASGR1 remains an independent influencing factor for hs-CRP and WBC count among individuals with CAD even after adjusting for lipid parameters (Table 3). Notably, patients without CAD did not exhibit this association (Tables 4 and 5). Thus, our findings suggest a potential connection between serum sASGR1 and inflammation in patients with CAD, independent of lipid metabolism disorders. This hypothesis has actually received indirect support from earlier studies. For instance, sialylation mediated by α2,3-sialyltransferases has been linked to the recruitment of circulating inflammatory myeloid cells to the atherosclerotic vascular endothelium [22, 48, 49]. Moreover, sASGR1 levels and monocyte counts were positively correlated according to the multivariate regression model (model III: β = 0.009, p = 0.014). ASGR1 is expressed in peripheral blood monocytes [50]. These findings suggest that, in addition to being secreted by hepatocytes, serum sASGR1 may also be secreted by monocytes. In summary, the positive correlation between the serum sASGR1 concentration and inflammatory marker (hs-CRP and WBC) levels in CAD patients supports the current view that ASGR1 is a risk factor for CAD. In addition, our research provides a reference for revealing the potential role of sASGR1 in the inflammation of atherosclerosis.
Study strengths and limitations
This is the first study in which we investigated the relationship between serum sASGR1 levels and CAD incidence, as well as inflammatory marker levels. This study has several limitations. First, this was a cross-sectional investigation, and the causal relationships between the serum sASGR1 concentration and CAD incidence or inflammatory marker levels could not be determined. However, further studies are needed to reveal the role of ASGR1 in the inflammation of atherosclerosis. Second, a relatively small sample size may hinder the ability to identify minute differences, even though the results of sample size calculations show that our sample size is appropriate for the main purpose of the study. These findings need to be confirmed in larger-sample studies. Third, the method of dividing the patients into groups with and without CAD may have resulted in selection bias. Fourth, we did not perform Western blot analysis of the serum sASGR1 concentration to confirm that this parameter is a biomarker for CAD, as suitable antibodies were not found. Finally, we did not investigate the correlation between sASGR1 levels and the levels of other inflammatory cytokines, such as ILs.
Conclusions
Our study suggested that serum sASGR1 levels are elevated in CAD patients and may be an independent risk factor for CAD. Moreover, sASGR1 was independently and positively correlated with inflammatory marker levels in CAD patients, even after controlling for lipid parameters. The potential role of sASGR1 in inflammation in atherosclerosis, independent of cholesterol metabolism, may need further study.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- ASGR1:
-
Asialoglycoprotein receptor 1
- CAD:
-
Coronary artery disease
- sASGR1:
-
Soluble ASGR1
- hASGR1:
-
Hepatic ASGR1
- Hs-CRP:
-
High-sensitivity CRP
- WBCC:
-
White blood cell count
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- VCAM:
-
Vascular cell adhesion molecule-1
- ICAM:
-
Intercellular adhesion molecule-1
- MCP-1:
-
Monocyte chemotactic protein-1
- APO-B:
-
Apolipoprotein B
- APO-A1:
-
Apolipoprotein A1
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- Lp(a):
-
Lipoprotein (a)
- IL-1:
-
Interleukin-1
- TNF-α:
-
Tumor necrosis factor
- EGFR:
-
Epidermal growth factor receptor
- AMI:
-
Acute myocardial infarction
- T2DM:
-
Type 2 Diabetes Mellitus
- BMI:
-
Body mass index
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- ELISA:
-
Enzyme-linked immunosorbent assay
- CI:
-
Confidence interval
References
Libby P. The changing nature of atherosclerosis: what we thought we knew, what we think we know, and what we have to learn. Eur Heart J. 2021;42(47):4781–2.
Tibaut M, Caprnda M, Kubatka P, Sinkovic A, Valentova V, Filipova S, et al. Markers of atherosclerosis: part 1 - serological markers. Heart Lung Circ. 2019;28(5):667–77.
Tibaut M, Caprnda M, Kubatka P, Sinkovic A, Valentova V, Filipova S, et al. Markers of atherosclerosis: part 2 - genetic and imaging markers. Heart Lung Circ. 2019;28(5):678–89.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72.
Della CV, Todaro F, Cataldi M, Tuttolomondo A. Atherosclerosis and its related laboratory biomarkers. Int J Mol Sci. 2023;24(21).
Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, et al. Atherosclerosis Nat Rev Dis Primers. 2019;5(1):56.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular Risk reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019;380(1):11–22.
Nordestgaard BG. Triglyceride-Rich lipoproteins and Atherosclerotic Cardiovascular Disease: New insights from Epidemiology, Genetics, and Biology. Circ Res. 2016;118(4):547–63.
Stone PH, Libby P, Boden WE. Fundamental pathobiology of coronary atherosclerosis and clinical implications for chronic ischemic heart Disease Management-the Plaque hypothesis: a narrative review. Jama Cardiol. 2023;8(2):192–201.
Sarraju A, Nissen SE. Atherosclerotic plaque stabilization and regression: a review of clinical evidence. Nat Rev Cardiol. 2024.
Yang S, Koo BK, Hoshino M, Lee JM, Murai T, Park J, et al. CT angiographic and plaque predictors of functionally significant Coronary Disease and Outcome using machine learning. JACC Cardiovasc Imaging. 2021;14(3):629–41.
Lee JM, Choi KH, Koo BK, Park J, Kim J, Hwang D, et al. Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J Am Coll Cardiol. 2019;73(19):2413–24.
Severino P, D’Amato A, Pucci M, Infusino F, Adamo F, Birtolo LI et al. Ischemic heart Disease Pathophysiology paradigms overview: from plaque activation to Microvascular Dysfunction. Int J Mol Sci. 2020;21(21).
Libby P. Inflammation during the life cycle of the atherosclerotic plaque. Cardiovasc Res. 2021;117(13):2525–36.
Libby P. Inflammation in Atherosclerosis-No longer a theory. Clin Chem. 2021;67(1):131–42.
Ashwell G, Harford J. Carbohydrate-specific receptors of the liver. Annu Rev Biochem. 1982;51:531–54.
Ashwell G, Morell AG. The role of surface carbohydrates in the hepatic recognition and transport of circulating glycoproteins. Adv Enzymol Relat Areas Mol Biol. 1974;41(0):99–128.
Spiess M. The asialoglycoprotein receptor: a model for endocytic transport receptors. Biochemistry-Us. 1990;29(43):10009–18.
Stockert RJ. The asialoglycoprotein receptor: relationships between structure, function, and expression. Physiol Rev. 1995;75(3):591–609.
Trowbridge IS, Collawn JF, Hopkins CR. Signal-dependent membrane protein trafficking in the endocytic pathway. Annu Rev Cell Biol. 1993;9:129–61.
Wang JQ, Li LL, Hu A, Deng G, Wei J, Li YF, et al. Inhibition of ASGR1 decreases lipid levels by promoting cholesterol excretion. Nature. 2022;608(7922):413–20.
Nioi P, Sigurdsson A, Thorleifsson G, Helgason H, Agustsdottir AB, Norddahl GL, et al. Variant ASGR1 Associated with a reduced risk of coronary artery disease. N Engl J Med. 2016;374(22):2131–41.
Hamledari H, Sajjadi SF, Alikhah A, Boroumand MA, Behmanesh M. ASGR1 but not FOXM1 expression decreases in the peripheral blood mononuclear cells of diabetic atherosclerotic patients. J Diabetes Complications. 2019;33(8):539–46.
Nakaya R, Kohgo Y, Mogi Y, Nakajima M, Kato J, Niitsu Y. Regulation of asialoglycoprotein receptor synthesis by inflammation-related cytokines in HepG2 cells. J Gastroenterol. 1994;29(1):24–30.
Liu Y, Zhu L, Liang S, Yao S, Li R, Liu S, et al. Galactose protects hepatocytes against TNF-alpha-induced apoptosis by promoting activation of the NF-kappaB signaling pathway in acute liver failure. Lab Invest. 2015;95(5):504–14.
Lu Q, Liu J, Zhao S, Gomez CM, Laurent-Rolle M, Dong J, et al. SARS-CoV-2 exacerbates proinflammatory responses in myeloid cells through C-type lectin receptors and Tweety family member 2. Immunity. 2021;54(6):1304–19.
Shi R, Wang J, Zhang Z, Leng Y, Chen AF. ASGR1 promotes liver injury in sepsis by modulating monocyte-to-macrophage differentiation via NF-kappaB/ATF5 pathway. Life Sci. 2023;315:121339.
Qu WS, Tian DS, Guo ZB, Fang J, Zhang Q, Yu ZY, et al. Inhibition of EGFR/MAPK signaling reduces microglial inflammatory response and the associated secondary damage in rats after spinal cord injury. J Neuroinflammation. 2012;9:178.
Li N, McLaren JE, Michael DR, Clement M, Fielding CA, Ramji DP. ERK is integral to the IFN-gamma-mediated activation of STAT1, the expression of key genes implicated in atherosclerosis, and the uptake of modified lipoproteins by human macrophages. J Immunol. 2010;185(5):3041–8.
Liu J, Hu B, Yang Y, Ma Z, Yu Y, Liu S, et al. A new splice variant of the major subunit of human asialoglycoprotein receptor encodes a secreted form in hepatocytes. PLoS ONE. 2010;5(9):e12934.
Luo Q, Chen J, Su Y, Wu P, Wang J, Fang Z, et al. Correlation between serum soluble ASGR1 concentration and low-density lipoprotein cholesterol levels: a cross-sectional study. Lipids Health Dis. 2023;22(1):142.
Arroyo-Espliguero R, Avanzas P, Cosin-Sales J, Aldama G, Pizzi C, Kaski JC. C-reactive protein elevation and disease activity in patients with coronary artery disease. Eur Heart J. 2004;25(5):401–8.
Ridker PM, Bhatt DL, Pradhan AD, Glynn RJ, MacFadyen JG, Nissen SE. Inflammation and cholesterol as predictors of cardiovascular events among patients receiving statin therapy: a collaborative analysis of three randomized trials. Lancet. 2023;401(10384):1293–301.
Ridker PM, Lei L, Louie MJ, Haddad T, Nicholls SJ, Lincoff AM, et al. Inflammation and cholesterol as predictors of Cardiovascular events among 13970 contemporary high-risk patients with statin intolerance. Circulation. 2024;149(1):28–35.
Ortega E, Gilabert R, Nunez I, Cofan M, Sala-Vila A, de Groot E, et al. White blood cell count is associated with carotid and femoral atherosclerosis. Atherosclerosis. 2012;221(1):275–81.
Madjid M, Fatemi O. Components of the complete blood count as risk predictors for coronary heart disease: in-depth review and update. Tex Heart Inst J. 2013;40(1):17–29.
Hasegawa T, Negishi T, Deguchi M. WBC count, atherosclerosis and coronary risk factors. J Atheroscler Thromb. 2002;9(5):219–23.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618–51.
Varbo A, Benn M, Tybjaerg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128(12):1298–309.
Yang G, Schooling CM. Genetically mimicked effects of ASGR1 inhibitors on all-cause mortality and health outcomes: a drug-target mendelian randomization study and a phenome-wide association study. Bmc Med. 2023;21(1):235.
Mazidi M, Wright N, Yao P, Kartsonaki C, Millwood IY, Fry H, et al. Plasma proteomics to identify drug targets for ischemic heart disease. J Am Coll Cardiol. 2023;82(20):1906–20.
Koba S, Hirano T, Ito Y, Tsunoda F, Yokota Y, Ban Y, et al. Significance of small dense low-density lipoprotein-cholesterol concentrations in relation to the severity of coronary heart diseases. Atherosclerosis. 2006;189(1):206–14.
Li S, Guo YL, Zhao X, Zhang Y, Zhu CG, Wu NQ, et al. Novel and traditional lipid-related biomarkers and their combinations in predicting coronary severity. Sci Rep. 2017;7(1):360.
Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation. 2000;102(18):2165–8.
Verma S, Wang CH, Li SH, Dumont AS, Fedak PW, Badiwala MV, et al. A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation. 2002;106(8):913–9.
Danenberg HD, Szalai AJ, Swaminathan RV, Peng L, Chen Z, Seifert P, et al. Increased thrombosis after arterial injury in human C-reactive protein-transgenic mice. Circulation. 2003;108(5):512–5.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with Canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31.
Frommhold D, Ludwig A, Bixel MG, Zarbock A, Babushkina I, Weissinger M, et al. Sialyltransferase ST3Gal-IV controls CXCR2-mediated firm leukocyte arrest during inflammation. J Exp Med. 2008;205(6):1435–46.
Doring Y, Noels H, Mandl M, Kramp B, Neideck C, Lievens D, et al. Deficiency of the sialyltransferase St3Gal4 reduces Ccl5-mediated myeloid cell recruitment and arrest: short communication. Circ Res. 2014;114(6):976–81.
Harris RL, van den Berg CW, Bowen DJ. ASGR1 and ASGR2, the genes that encode the Asialoglycoprotein receptor (Ashwell Receptor), are expressed in Peripheral Blood monocytes and Show Interindividual differences in transcript Profile. Mol Biol Int. 2012;2012:283974.
Acknowledgements
We would like to express our gratitude to all those who helped us during the writing of this manuscript.
Funding
This work was supported by the National Natural Science Foundation of China [grant number 82100495 to F. Luo, grant number 82201879 to J.F. Chen]; the Hunan Provincial Natural Science Foundation of China [grant number 2021JJ40852 to F. Luo, grant number 2022JJ40675 to J.F. Chen]; the Scientific Research Project of Hunan Provincial Health Commission [grant number 202203014009 to F. Luo, grant number B202305037231 to J.F. Chen]; the Scientific Research Launch Project for New Employees of the Second Xiangya Hospital of Central South University [to F. Luo and J.F. Chen]; the China Postdoctoral Science Foundation [grant number 331046 and 2023T160738 to F. Luo and J.F. Chen]; and the Key Research and Development Program of Hunan Province of China [grant number 2021SK2004 to Z.F. Fang].
Author information
Authors and Affiliations
Contributions
FL, ZF and QL conceived the idea. QL wrote the manuscript; JC, YY and PW conducted the data collection and analysis. FL, ZC, YS, HAA, JT and ZF read through and corrected the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the ethics committee of the Second Xiangya Hospital. Informed consent was obtained from each patient.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, Q., Chen, J., Yi, Y. et al. The serum soluble ASGR1 concentration is elevated in patients with coronary artery disease and is associated with inflammatory markers. Lipids Health Dis 23, 89 (2024). https://doi.org/10.1186/s12944-024-02054-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02054-8